This observational study from the CIBMTR® (Center for International Blood and Marrow Transplant Research®) evaluated the effectiveness of post-transplant cyclophosphamide (PTCy) for graft-versus-host disease (GVHD) prevention in recipients of human leukocyte antigen (HLA)-matched unrelated donor (8/8 MUD) and mismatched (7/8) unrelated donor (MMUD) hematopoietic cell transplantation (HCT).
Download a PDF of the study highlights and citation.
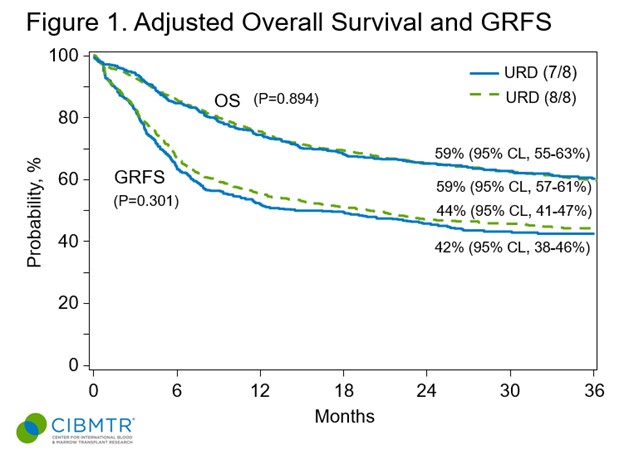
Findings suggest that the use of PTCy can eliminate disparities in survival between MUD and MMUD HCT, with MUD HCT still performing favorably over haplo HCT as a comparison group. The adoption of PTCy can greatly improve HCT outcomes while helping to expand access to those without a MUD available, which disproportionally impacts patients who are racially and ethnically diverse.
Background
PTCy has become an established standard approach for GVHD prevention. It has displayed efficacy across HLA mismatch barriers, expanding the possibilities for successful HCT regardless of a patient’s race or ethnicity. A previous clinical trial sponsored by NMDPSM found promising survival rates in adult patients receiving MMUD bone marrow grafts. NMDP is committed to exploring the differences in GVHD-free, relapse-free survival (GRFS) rates between various unrelated donor (URD) sources with the hopes of bridging any observed gaps.
Study Details
The study included 4,829 patients who underwent their first allogeneic HCT procedure between 2017 and 2020 to treat acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML) or myelodysplastic syndrome (MDS). Patients were given PTCy-based GVHD prophylaxis.
Of these patients, 1,517 were recipients of 8/8 MUDs, 540 were 7/8 MMUDs, and 2,772 were haploidentical (haplo) related donors. The MUD patients had a slightly different composition, with more patients having MDS and undergoing myeloablative conditioning compared to the other two groups. However, all groups were comparably balanced in terms of donor, patient and disease characteristics.
Results
Results indicated no notable differences in GRFS or overall survival (OS) between the recipients of 8/8 MUD and 7/8 MMUD HCT for up to 3 years post-HCT. The outcomes, including rates of relapse and non-relapse mortality (NRM), were consistent across these two groups, regardless of conditioning intensity. The study did find that MUD HCT was associated with a slightly reduced risk of moderate/severe chronic GVHD compared to 7/8 MMUD. When comparing MUD to haplo HCT, GRFS and OS were significantly better for the MUD group. This advantage was primarily attributed to the higher NRM and chronic GVHD rates observed in haplo transplants.
Interestingly, the 3-year comparison between 7/8 MMUD and haplo showed no significant difference in GRFS or OS. The main causes of death among donor types were relapse/progression of the primary disease, infections and organ failure.
Key Takeaways
PTCy-based GVHD prevention was found to minimize the observed disparities in GRFS and OS between 8/8 MUD and 7/8 MMUD HCT. MUD HCT remains the most favorable option for patients lacking a matched sibling donor since it offers superior GRFS and OS. Further studies are needed to compare haplo with 7/8 MMUD HCT, particularly with a larger MMUD sample size.
Employing PTCy-based GVHD prophylaxis dramatically reduces the risk associated with transplants across the HLA-mismatch barrier. The ability to use mismatched donors, thanks to PTCy, has significantly broadened the potential pool of donors, ensuring patients from diverse racial and ethnic backgrounds can access HCT.
Auletta JJ, et al., ASH oral presentation abstract.
