Timing Impact on Outcomes
In general, patients transplanted in earlier disease stages have better outcomes than patients transplanted in more advanced disease stages, regardless of the degree of HLA match. Because appropriate planning and early donor identification are critical in optimal outcomes, early consultation is appropriate, even for patients who do not go on to transplant.
Early Referral Can Improve Outcomes
Studies on hematopoietic cell transplantation (HCT) have revealed that transplant success can be highly dependent upon transplant timing. In a study of 8,003 unrelated donor transplants, patients with intermediate-stage disease had a 40% greater risk of mortality than patients with early-stage disease.
And at 3- and 5-years post-transplant, patients with early-stage disease experienced survival rates of more than twice the rates of patients with advanced disease: 56% vs. 27%, and 50% vs. 22%, respectively. [1, supplemental analysis by author] This study confirmed the results of an earlier study where researchers also concluded that early referral is perhaps the single most important step that can affect survival. [2]
Optimal Timing for Transplantation
For many diseases, research has identified the optimal timing for HCT:
- Patients with intermediate- or poor-risk acute myeloid leukemia (AML) in first complete remission (CR1) have significantly better relapse-free survival compared to consolidation chemotherapy and autologous transplant [3]
- If a transplant is indicated, early referral to prepare for transplant in CR1 is recommended in patients with intermediate- and poor-risk AML. [4,5,6]
- Short duration of CR in leukemia necessitates collaboration with transplant physicians early after diagnosis [7]
- Better outcomes are achieved when patients with myelodysplastic syndromes with intermediate or high IPSS scores undergo allogeneic HCT before they progress to advanced disease [8,9]
- In patients with severe aplastic anemia, earlier allogeneic HCT is preferred in order to avoid HLA-sensitization during transfusion [10]
- Infants with immunodeficiency disorders have better outcomes when transplanted <3.5 months of age and without active infections [11]
- Early transplantation improves outcomes in patients with inherited metabolic disorders, before organ and cognitive damage progresses [12,13]
- For patients with chemotherapy-sensitive mantle cell lymphoma, the optimal timing for HCT is early in the disease course [14]
Outcomes
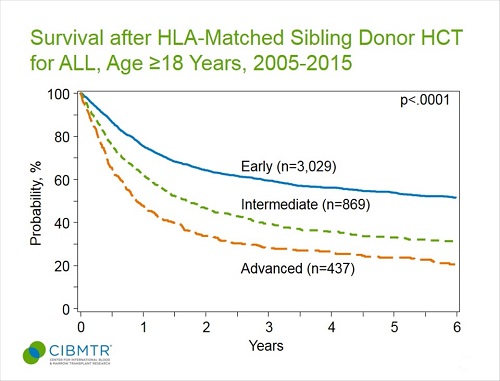
Outcomes for allogeneic transplantation in three patient populations are shown below, comparing outcomes by disease stage at time of transplantation. In each patient cohort, transplantation in earlier disease stage leads to significantly better survival compared to transplantation in later disease stage. Our outcomes by disease status slides illustrate this in several other patient populations.
Figure 1. AML, Survival of Adult Marrow Transplant Patients, by Disease Status
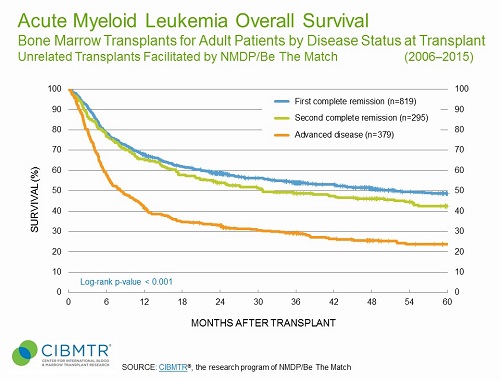
Figure 2. ALL, Survival of Pediatric Marrow Transplant Patients, by Disease Status
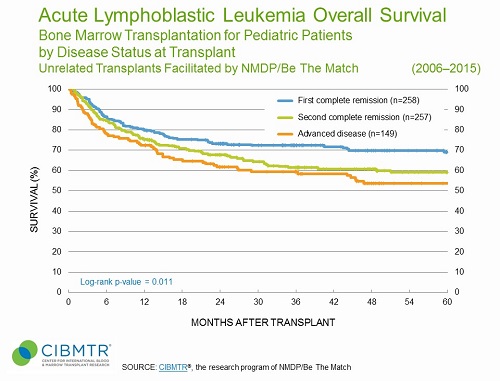
Figure 3. ALL, Survival of HLA-Identical Sibling Adult Transplants, by Disease Status
Data in this section have been prepared by CIBMTR® (Center for International Blood and Marrow Transplant Research®), a research collaboration between the National Marrow Donor Program®/Be The Match® and Medical College of Wisconsin.
Referral Timing Guidelines
Transplant Consultation Timing Guidelines
The National Marrow Donor Program® (NMDP)/Be The Match®, together with the American Society for Blood and Marrow Transplantation (ASBMT), have developed Recommended Timing for Transplant Consultation guidelines that identify the optimal timing for transplant consultation by disease. [15] These are available in print, online, and as a mobile app:
References
- Pidala J, Lee SJ, Ahn KW, et al. Nonpermissive HLA-DPB1 mismatch increases mortality after myeloablative unrelated allogeneic hematopoietic cell transplantation. Blood. 2014; 124(16): 2596-2606. Access
- Lee SJ, Klein J, Haagenson M, et al. High-resolution donor-recipient HLA matching contributes to the success of unrelated donor marrow transplantation. Blood. 2007; 110(13): 4576-4583. Access
- Koreth J, Schlenk R, Kopecky KJ, et al. Allogeneic stem cell transplantation for acute myeloid leukemia in first complete remission: Systematic review and meta-analysis of prospective clinical trials. JAMA. 2009; 301(22): 2349-2361. Access
- Michelis FV, Messner HA, Atenafu EG, et al. Benefit of allogeneic transplantation in patients age ≥60 years with acute myeloid leukemia is limited to those in first complete remission at time of transplant. Biol Blood Marrow Transplant. 2014; 20(4): 474-479. Access
- Döhner H, Weisdorf DJ, Bloomfield CD. Acute Myeloid Leukemia. N Engl J Med. 2015;373(12): 1136-1152. Access
- NCCN Clinical Practice Guidelines in Oncology. Acute Myeloid Leukemia Version 1.2015. Accessed January 5, 2016. Access
- Ustun C, Lazarus HM, Weisdorf D. To transplant or not: A dilemma for treatment of elderly AML patients in the twenty-first century. Bone Marrow Transplant. 2013; 48(12): 1497-1505. Access
- Koreth J, Pidala J, Perez WS, et al. Role of reduced-intensity conditioning allogeneic hematopoietic stem-cell transplantation in older patients with de novo myelodysplastic syndromes: An international collaborative decision analysis. J Clin Oncol. 2013; 31(21): 2662-2670. Access
- Alessandrino EP, Porta MG, Malcovati L, et al. Optimal timing of allogeneic hematopoietic stem cell transplantation in patients with myelodysplastic syndrome. Am J Hematol. 2013; 88(7): 581-588. Access
- Cutler C. Timing of allogeneic stem cell transplantation for myelodysplastic syndromes and aplastic anemia. Hematology Am Soc Hematol Edu Program. 2014; 2014: 77-81. Access
- Pai S-Y, Logan BR, Griffith LM, et al. Transplantation outcomes for severe combined immunodeficiency, 2000-2009. N Engl J Med. 2014; 371(5): 434-446. Access
- Aldenhoven M, Wynn RF, Orchard PJ, et al. Long-term outcome of Hurler syndrome patients after hematopoietic cell transplantation: An international multi-center study. Blood. 2015; 125(13): 2164-2172. Access
- Wynn R. Stem cell transplantation in inherited metabolic disorders. Hematology Am Soc Hematol Edu Program. 2011; 2011: 285-291. Access
- Fenske TS, Zhang M-J, Carreras J, et al. Autologous or reduced-intensity conditioning allogeneic hematopoietic cell transplantation for chemotherapy-sensitive mantle-cell lymphoma: Analysis of transplantation timing and modality. J Clin Oncol. 2014; 32(4): 273-281. Access