This observational study from CIBMTR® (Center for International Blood and Marrow Transplant Research®)—a research collaboration between the Medical College of Wisconsin® and NMDPSM—aimed to refine donor selection criteria for allogeneic hematopoietic cell transplantation (HCT) by evaluating the impact of donor characteristics on matched unrelated donor (MUD) HCT outcomes. The main finding highlights that donor age has significant effects on patient outcomes, with a preference for donors between 18 and 30 years old. Notably, results suggest that donors 18–30 years old may lead to similar outcomes with only negligible improvements with younger age, allowing for more flexibility when selecting an optional HCT donor. These insights could influence donor selection practices and expand the optimal donor pool.
Background
HLA matching has been pivotal in predicting successful unrelated donor HCT outcomes. Yet, the prioritization of equivalently matched donors based on additional characteristics like age, gender, and cytomegalovirus (CMV) status remains controversial. Previous studies suggested the youngest available donor as optimal but focused primarily on overall survival (OS) within a limited follow-up period. This study extends the analysis to both OS and event-free survival (EFS) over 3 years, employing advanced machine learning techniques to assess the influence of various donor characteristics.
Methods
The study analyzed over 11,800 first 8/8 MUD transplants reported to CIBMTR from 2016–2019, with a subset of 699 patients having detailed donor search data. Using Non-parametric failure time – Bayesian additive regression trees (NFT-BART), the research assessed the impact of donor age, gender, prior pregnancy, CMV status, and HLA-DQB1 or -DPB1 T-cell epitope (TCE) permissive matching on OS and EFS. The optimization of donor selection was explored through real-world data, considering different strategies to enhance OS and EFS.
Results
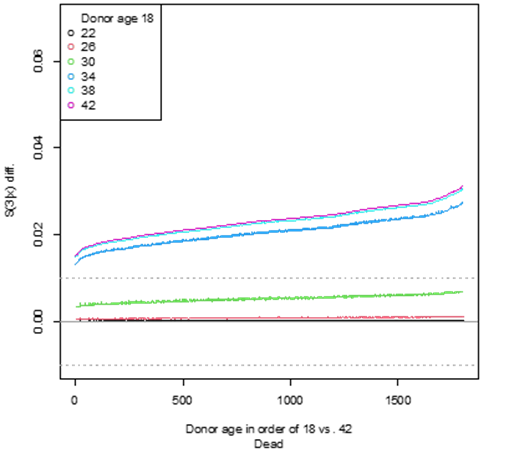
Analysis revealed that only donor age significantly affects OS and EFS, offering substantial benefits when comparing an 18-year-old donor to those aged 34 and above. Notably, the study found minimal impact on outcomes when choosing among donors aged 18 to 30, suggesting flexibility in donor selection within this age range. Gender showed a minor effect, favoring male donors for EFS when age differences were minimal. An optimization strategy balancing OS and EFS confirmed the potential for nuanced donor selection, prioritizing OS while considering EFS when differences in OS are marginal. CMV status, donor parity, HLA-DQB1 matching and HLA-DPB1 TCE permissive/non-permissive matching did not impact OS or EFS in this analysis.
Key Takeaways
The study highlights the importance of donor age in allogeneic HCT outcomes, suggesting a range of optimal MUD donor ages (18–30 years) that allow for flexibility in selection. This insight provides a foundation for updated guidelines in donor selection, potentially expanding the donor pool and improving the likelihood of successful transplantation outcomes for patients.
Figure
This figure displays predicted OS differences at 3 years post-transplant for an 18-year-old vs. an older donor considering donors aged 22, 26, 30, 34, 38 and 42 years old. Compared to donors 34 and older, an 18-year-old is associated with a substantial increase in OS (>1%) at 3 years. Compared to donors 22 to 30, an 18-year-old choice produces benefits that are negligible (<1% improvement in OS at 3 years).
Sparapani RA, et al., ASH abstract published in Blood
