Acute Myeloid Leukemia (AML) - Adult
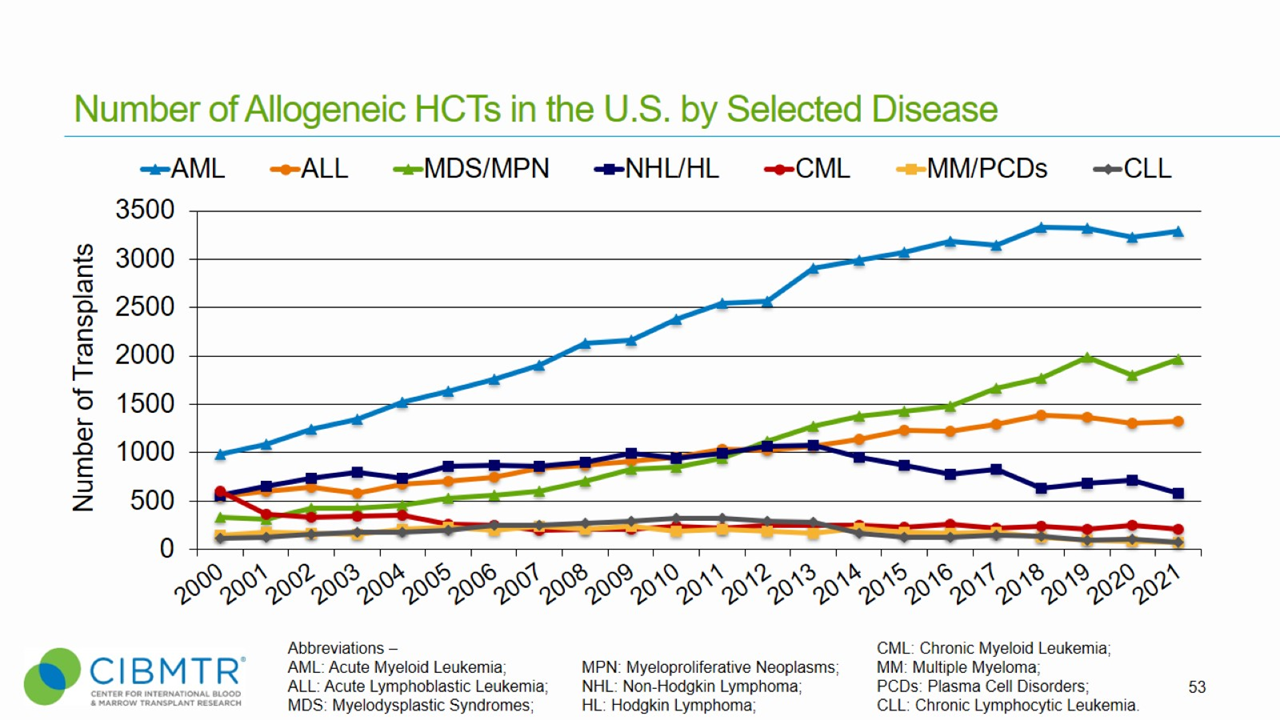
Allogeneic stem cell transplantation is an important treatment option in the management of adult acute myeloid leukemia (AML). [1] Worldwide, physicians perform more than 7,000 allogeneic transplants for AML, making it the most common and fastest growing indication for allogeneic HCT. [2]
Recent advances informing clinical decision-making include increasing identification of prognostic genetic markers in AML used to determine the disease risk status and a composite comorbidity/age score for treatment risk stratification. [1-8]
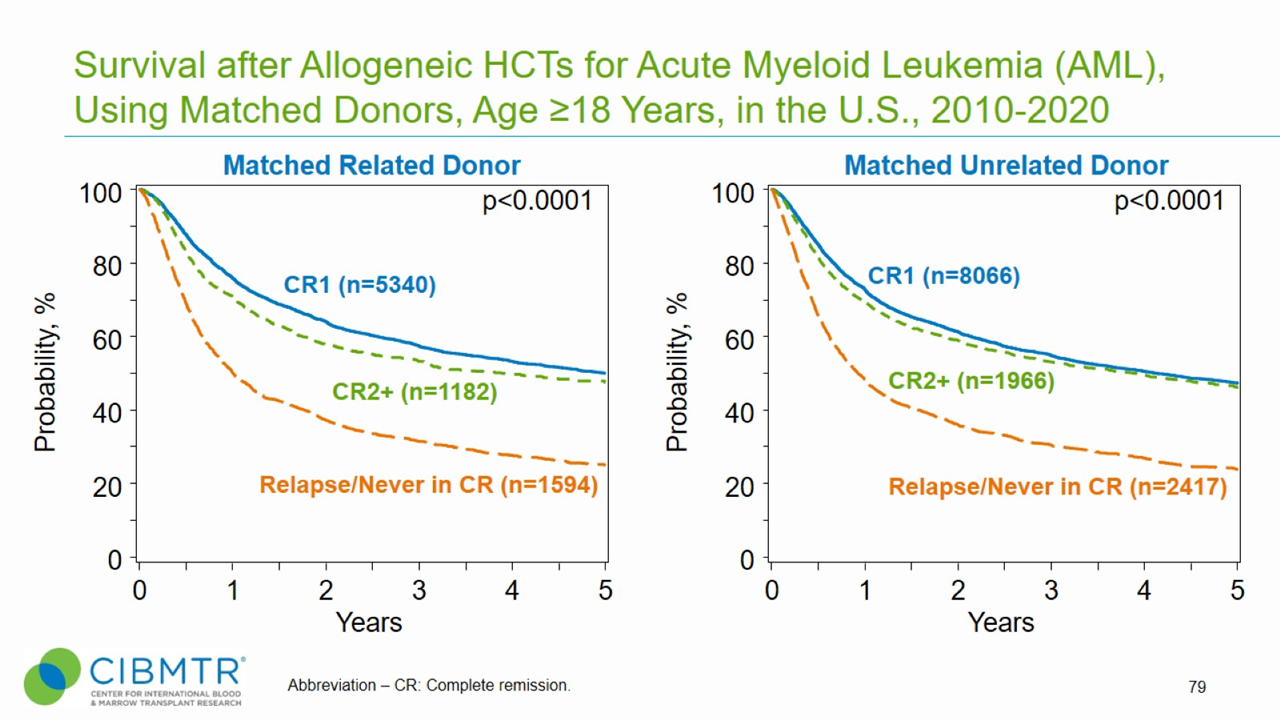
Because of these advances, more is known about which patients are eligible for hematopoietic cell transplantation (HCT) and which are not. In addition, large-scale studies have determined the optimal timing for HCT. As shown in Figure 1, patients with AML transplanted while in first or second complete remission have significantly better outcomes than patients transplanted with advanced disease. This is true whether the patient is undergoing matched related or matched unrelated HCT.
Figure 1. Survival Over Time, Matched Related and Matched Unrelated HCT for AML
As shown in Figure 2, increasing numbers of patients over age 64 years are undergoing HCT, which is due to reduced-intensity conditioning regimens and better post-transplant supportive care.
Figure 2. Trend of Allogeneic HCT for Malignant Diseases in Adult and Pediatric Recipients
Recent research shows an upper age limit may not be a barrier to allogeneic HCT for patients with AML. A CIBMTR® study published in Bone Marrow Transplantation showed differences in outcomes among patient groups were better associated with covariates, such as comorbidities and immunosuppression regimen, than age. Research suggests that patient age alone should not be considered exclusion criteria for a transplant consultation. [9]
For patients with intermediate- and poor-risk cytogenetics, a meta-analysis demonstrated a survival benefit of allogeneic HCT in first complete remission over chemotherapy. [10] Early referral for HCT evaluation for these at-risk patients at an early disease stage can significantly improve survival. [11,12]
Outcomes
Data in this section have been prepared by the CIBMTR. The CIBMTR is a research collaboration between the National Marrow Donor Program® (NMDP)/Be The Match® and the Medical College of Wisconsin.
Figure 3. AML Survival, Haploidentical and Mismatched Unrelated Adult Allogeneic HCT
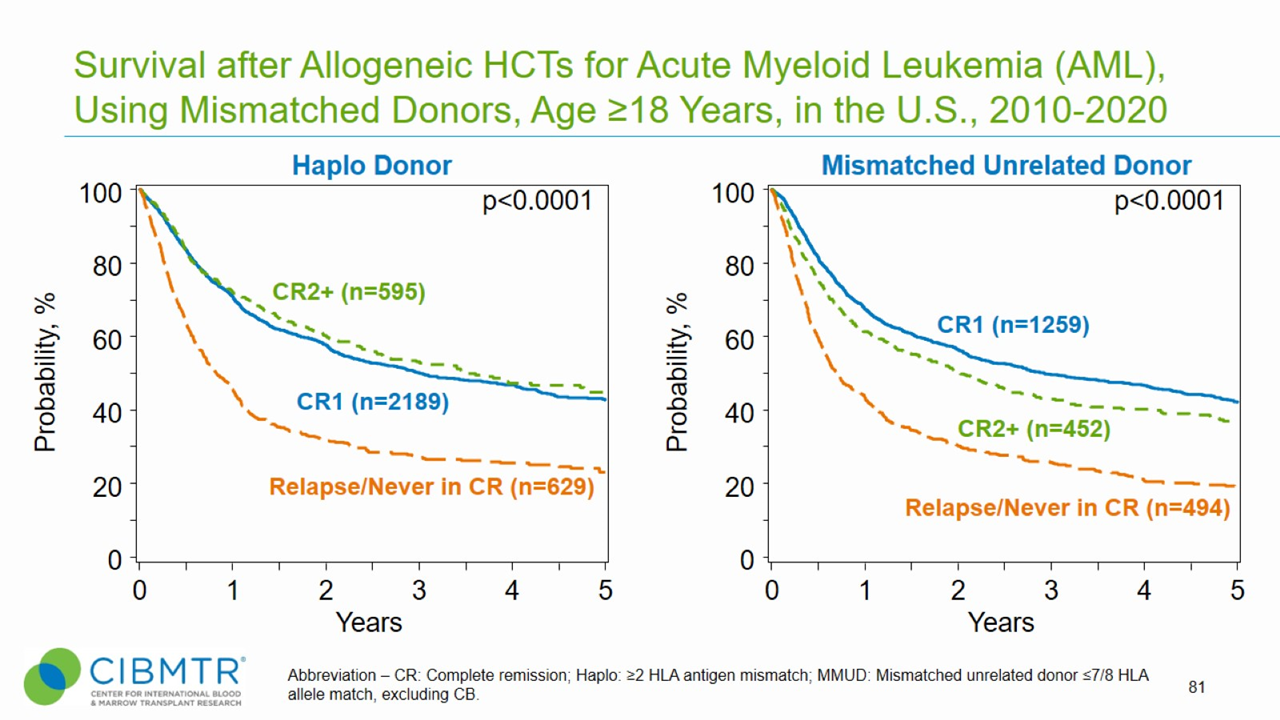
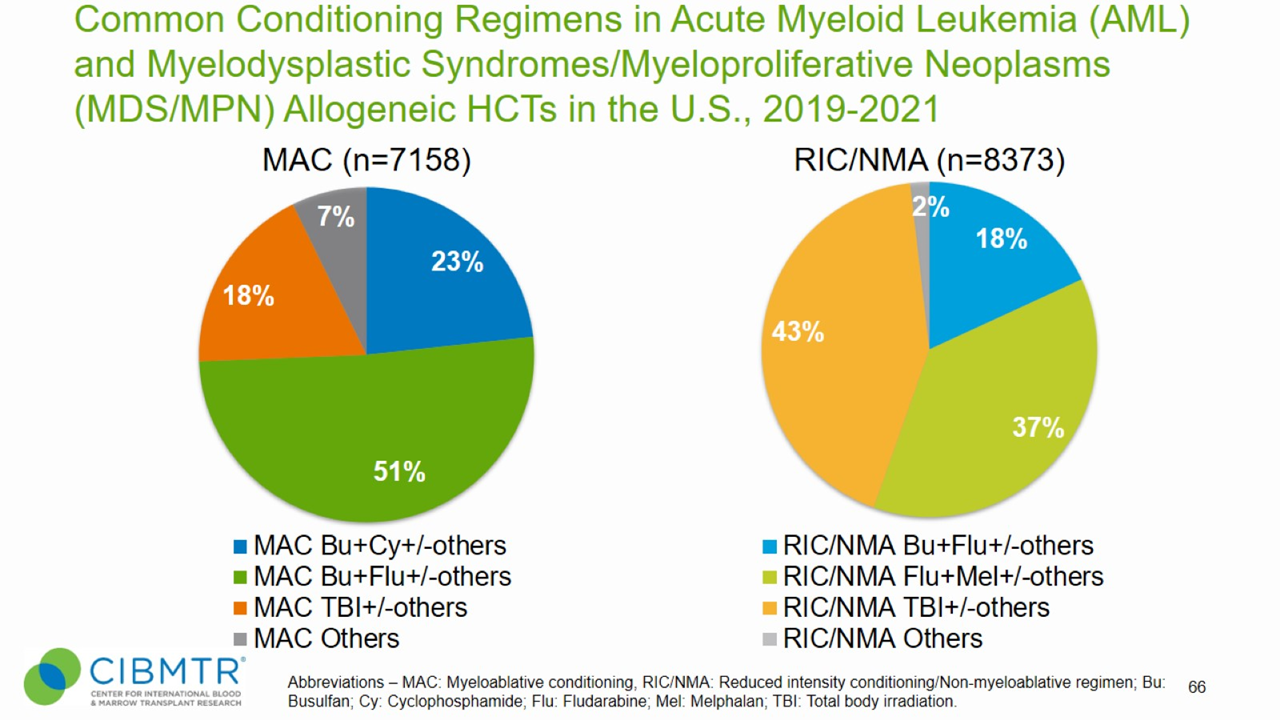
Figure 4. Conditioning Regimens in AML and Myelodysplastic Syndromes/Myeloproliferative Neoplasms, Allogeneic HCT
HCT Consultation Timing Guidelines
The National Marrow Donor Program® (NMDP)/Be The Match® and the American Society for Transplantation and Cellular Therapy (ASTCT) have jointly developed guidelines for transplant consultation and referral timing based on disease characteristics. [13] The National Comprehensive Cancer Network Clinical Practice Guidelines (NCCN Guidelines®) were consulted when developing these guidelines and are a valuable tool in determining risk stratification. [14]
Our guidelines highlight disease categories that include patients at risk for disease progression and who should be referred for a consultation for autologous or allogeneic transplantation. [13]
Transplant Consultation Guidelines: Adult AML
High-resolution HLA typing is recommended at diagnosis for all patients
HCT consultation should take place early after initial diagnosis for all patients with AML, including:
- Primary induction failure
- Measurable (also known as minimal) residual disease after initial therapy
- CR1 - except favorable risk AML [defined as: t(8;21)(q22;q22.1); RUNX1-RUNX1T1, inv(16)(p13.1q22) or t(16;16)(p13.1;q22); CBFB-MYH11, mutated NPM1 without FLT3-ITD, biallelic mutated
- Early referral for allogeneic HCT should be considered for any patient with AML in CR1 who is 60 years or older, regardless of cytogenetic or genomic information
- Antecedent hematological disease (e.g., myelodysplastic syndrome [MDS])
- Treatment-related leukemia
- First relapse
- CR2 and beyond, if not previously evaluated
View complete HCT Consultation Timing Guidelines
Clinical Trials Search and Support
The NMDP/Be The Match offers the Be The Match® Jason Carter Clinical Trials Search and Support (CTSS) program, which can provide clinical trial navigation to your patients. The CTSS Program was created to help people with blood cancers or blood disorders and their families find and join clinical trials.
For more information, visit Clinical Trials Search and Support.
References
- Vyas P, Appelbaum FR, Craddock C. Allogeneic hematopoietic cell transplantation for acute myeloid leukemia. Biol Blood Marrow Transplant. 2015; 21(1): 8-15. Access
- Gratwohl A, Baldomero H, Aljurf M, et al. Hematopoietic stem cell transplantation: A global perspective. JAMA. 2010; 303(16): 1617-1624. Access
- Patel JP, Gönen M, Figueroa ME, et al. Prognostic relevance of integrated genetic profiling in acute myeloid leukemia. N Engl J Med. 2012; 366(12): 1079-1089. Access
- Röllig C, Bornhäuser M, Kramer M. et al. Allogeneic stem-cell transplantation in patients with NPM1-mutated acute myeloid leukemia: Results from a prospective donor versus no-donor analysis of patients after upfront HLA typing within the SAL-AML 2003 trial. J Clin Oncol. 2015; 33(5): 403-410. Access
- Ofran Y, Rowe JM. Genetic profiling in acute myeloid leukaemia – where are we and what is its role in patient management. Br J Haematol. 2013; 160(3): 302-320. Access
- Döhner H, Estey E, Grimwade D, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017; 129(4): 424-447. Access
- Schlenk RF, Kayser S, Bullinger L, et al. Differential impact of allelic ratio and insertion site in FLT3-ITD-positive AML with respect to allogeneic transplantation. Blood. 2014; 124(23): 3441-3449. Access
- Sorror ML, Storb RF, Sandmaier BM, et al. Comorbidity-age index: A clinical measure of biologic age before allogeneic hematopoietic cell transplantation. J Clin Oncol. 2014; 32(29): 3249-3256. Access
- Maakaron, J.E., Zhang, MJ., Chen, K. et al. Age is no barrier for adults undergoing HCT for AML in CR1: contemporary CIBMTR analysis. Bone Marrow Transplant. 2022:57: 911–917. Access
- Koreth J, Schlenk R, Kopecky KJ, et al. Allogeneic stem cell transplantation for acute myeloid leukemia in first complete remission: Systematic review and meta-analysis of prospective clinical trials. JAMA. 2009; 301(22): 2349-2361. Access
- Pidala J, Lee SJ, Ahn KW, et al. Nonpermissive HLA-DPB1 mismatch increases mortality after myeloablative unrelated allogeneic hematopoietic cell transplantation. Blood. 2014; 124(16): 2596-2606. Access
- Lee SJ, Klein J, Haagenson M, et al. High-resolution donor-recipient HLA matching contributes to the success of unrelated donor marrow transplantation. Blood. 2007; 110(13): 4576-4583. Access
- NMDP/Be The Match and ASTCT Recommended Timing for Transplant Consultation. Download (PDF)
- National Comprehensive Cancer Network. Acute Myeloid Leukemia. (Version 2.2022). Access