A shared care model between hematology/oncology practices and transplant centers showed few differences in outcomes compared to the usual care model for patients post-allogeneic hematopoietic cell transplantation (HCT).
According to research presented at the 64th American Society of Hematology (ASH) Annual Meeting and Exposition, non-relapse mortality (NRM) and overall survival (OS) at day 100 post-transplant were not significantly different between groups. Quality of life (QOL) at day 180 post-HCT did not show significant differences; however, patients in the shared care group reported significantly better QOL scores at day 100.
Results suggest that shared care may have the potential to become a new standard for safe and effective follow-up care after HCT.
Background
Methodological advances and improvements in supportive care have increased the number of patients eligible for HCT. However, accessibility remains an issue in the United States because most patients don’t reside close to a transplant center. The need for specialized follow-up in the months after transplant can cause a substantial burden on the patient’s finances, caregivers, and QOL.
A way to alleviate the strain is to allow local hematologic oncologists to provide some elements of post-HCT care closer to patients. Post-HCT care is complex, and it’s unknown if care can safely be shared among transplant centers and local providers without compromising outcomes.
Study Details
This randomized controlled trial from December 2017 to December 2021 included 302 HCT patients, 152 randomized in the shared care model group and 150 in the usual care model group. The median age was 63 with similar baseline characteristics across groups. Patients enrolled were referred to Dana-Farber Cancer Institute (DFCI) from 8 local hematology/oncology practices.
The shared care model involved four care delivery strategies allowing patients to be seen safely by local providers after HCT. The strategies included a formal online care coordination plan, patient engagement and education, local physician engagement and education (including yearly face-to-face training with DFCI transplant physicians), and a shared patient-physician-transplanter web portal and communication platform.
Patients alternated follow-up visits between the local site and the DFCI through day 100 with the shared care arm but exclusively visited DFCI in the usual care arm.
Results
At day 100 post-HCT, NRM and OS showed minimal differences, along with similar rates of acute graft-versus-host disease between both groups, as shown in Figure 1. There were no significant differences in QOL between groups at day 180 post-HCT; however, at day 100 post-HCT, the shared care group reported significantly better outcomes than the usual care group on QOL surveys.
QOL values on FACT-BMT surveys that were better in the shared care group on day 100 post-HCT included physical well-being, emotional well-being and bone marrow transplantation subscales. The QLQ-C30 survey at day 100 showed global, emotional, cognitive, fatigue, nausea and dyspnea scores were better in the shared care group.
Key Takeaways
When compared to usual care, shared care with local providers after HCT did not compromise day 100 NRM or day 180 QOL outcomes. Many QOL scores at day 100 post-transplant were significantly better in the shared care group compared to the usual care group.
These data suggest shared care could be a safe option for a new standard of transplant follow-up to alleviate transplant center and patient burden post-HCT and allow for more treatment to occur closer to home for patients. Implementation of a shared care model should include strict adherence to the four care delivery strategies and may improve access and quality of life for patients needing HCT.
Figure 1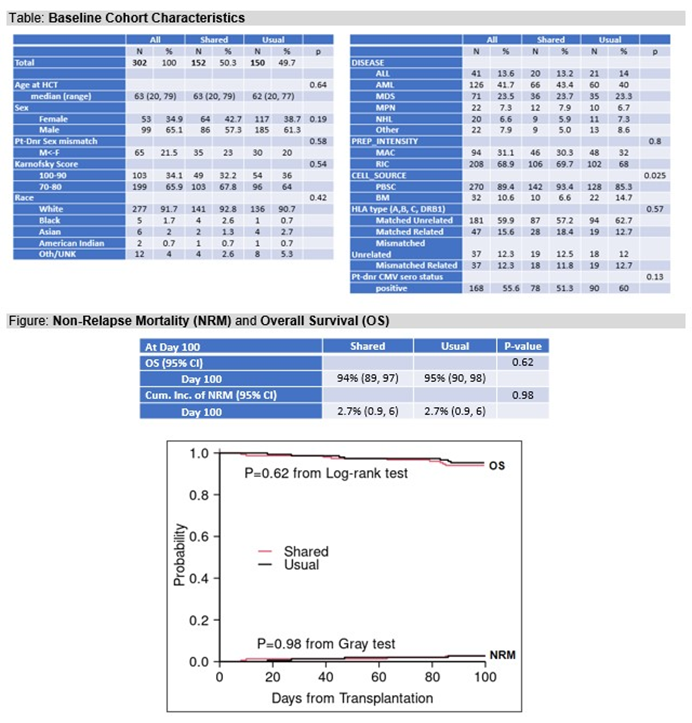
Abel GA, et al., ASH oral presentation abstract
