An observational research study presented at the 2023 Tandem Meetings of ASTCTTM and the CIBMTR® showed that when a matched sibling donor (MSD) is unavailable, alternative donor sources may be comparable to haploidentical (haplo) donors as a viable option for patients with myelofibrosis needing allogeneic hematopoietic cell transplantation (alloHCT). Patient outcomes 3 months post-transplant showed no statistically significant difference in overall survival (OS), non-relapse mortality (NRM), disease-free survival (DFS), and relapse between any of the four donor sources reviewed.
Background
A previous study comparing donor sources for patients with myelofibrosis demonstrated superior outcomes when using MSD versus matched unrelated donor (MUD) HCT. However, this was conducted before the more widespread use of haplo-related donors as an alternative donor source using post-transplant cyclophosphamide (PTCy). The use of haplo for myelofibrosis patients is growing, but studies comparing outcomes between MSD, MUD, mismatched unrelated donor (MMUD), and haplo HCT are lacking.
Study Details
The CIBMTR Chronic Leukemia Working Committee used data from the CIBMTR research database for this study. The study cohort included 1,057 adult patients (18 years and older) receiving a first alloHCT using peripheral blood stem cell grafts from MSD, MUD, MMUD, or haplo donors to treat chronic phase myelofibrosis from 2013 through 2019. Recipients of MUD HCT were fully matched (8/8), MMUD HCT were single mismatched (7/8), and haplo HCT were mismatched (<=6/8) at high resolution. The median follow-up for haplo HCT was shorter than the other groups (36 vs. 46-49 months). The primary outcome was OS, and secondary outcomes were relapse, NRM, and DFS.
Results
Patients across all donor groups were similar in age and gender. Patients receiving haplo HCT with PTCy were more ethnically diverse (40% vs. 10-24%) and received more reduced-intensity conditioning regimens (72% vs. 55% and lower). PTCy-based graft-versus-host disease (GVHD) prophylaxis occurred in the haplo HCT group but only in a small percentage of the other donor groups.
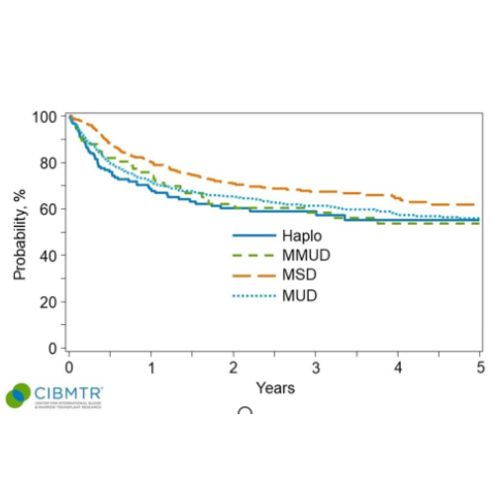
OS in the first 3 months was better for MSD recipients, mostly due to lower NRM with MSD HCT. Patients alive after 3 months post-transplant did not have a statistically significant difference in OS, NRM, relapse, or DFS between any donor type. The probability of OS at 3 years post-transplant was comparable between groups (haplo 58%, MSD 68%, MUD 62%, and MMUD 58%), as shown in Figure 1.
Key Takeaways
MSD is the preferred donor in patients with myelofibrosis when available. However, for many patients lacking an MSD, haplo HCT with PTCy for GVHD prevention has shown to be a comparable option to unrelated donors receiving the standard of care GVHD prevention using a calcineurin inhibitor. A recent study showing outcomes of a novel three-drug combination, including PTCy, may change the standard of care GVHD prevention strategy and warrants future research. In addition, alternative donors have shown to be a safe option for myelofibrosis patients, which should reduce access barriers to transplantation.
Figure 1. Survival Probability by Donor Type
Jain T, et al., Tandem Abstract
