Planned cryopreservation of allogeneic hematopoietic cell transplantation (HCT) grafts did not adversely impact early post-HCT outcomes in a study presented at the 63rd American Society of Hematology (ASH) Annual Meeting and Exposition. The shift in clinical practice to cryopreserved products necessitated during the COVID-19 pandemic was not found to have adversely impacted early (about 6 months) post-transplant survival or risk of primary graft failure.
Download a PDF of the full study summary with journal citation here: Research Brief
During the COVID-19 pandemic, concerns regarding travel logistics and donor safety necessitated a substantial increase in the use of cryopreserved HCT grafts from both related and unrelated donors to ensure graft availability prior to the start of conditioning. However, pre-pandemic data beyond single center or small multi-center reports are conflicting, lacking, and therefore have been unable to reassure clinicians that cryopreservation does not adversely impact post-HCT outcomes. Researchers sought to evaluate early post-HCT clinical outcomes in patients reported to the CIBMTR® (Center for International Blood and Marrow Transplant Research®) database who received a first allogeneic HCT using cryopreserved grafts at the height of the pandemic. The CIBMTR is a research collaboration between the National Marrow Donor Program®/Be The Match® and Medical College of Wisconsin.
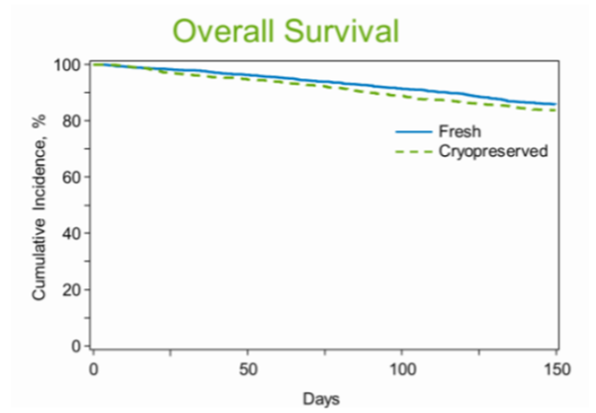
Hematopoietic engraftment and overall survival (OS) of patients receiving cryopreserved grafts between March and August of 2020 were compared to patients allografted using fresh products transplanted between March through August of 2019. The study included data from the CIBMTR database from 959 recipients of cryopreserved products and 2,499 recipients of fresh products from matched related or unrelated donors.
No impact of cryopreservation on OS was detected. Median time to neutrophil (a measure of how your immune system is functioning) and platelet engraftment were both delayed by one day in recipients of cryopreserved grafts, but there was no difference in the risk of primary graft failure by Day 28. Some delay in Day 100 platelet engraftment was observed in recipients of cryopreserved grafts, but there were no interactions identified between donor or graft type for OS or engraftment. Other important clinical outcomes such as secondary graft failure, acute GVHD and early relapse continue to be analyzed.
Researchers concluded that the shift in clinical practice to cryopreserved products necessitated during the pandemic did not adversely impact post HCT OS or risk of primary graft failure. It will, however, be critical to follow the cohort studied and subsequent recipients of cryopreserved grafts for much longer periods to determine the ultimate impact of cryopreservation on outcomes. Nevertheless, this large multi-center study will be useful to inform clinical decision making both during and following the pandemic. Safe and effective use of planned cryopreservation increases flexibility in donor collection scheduling, helping to eliminate barriers to donation based on transplant schedule.
Overall Survival