According to research published in Transplantation and Cellular Therapy, HLA-matched unrelated donor (MUD) and matched sibling donor (MSD) hematopoietic cell transplantation (HCT) showed superior outcomes over haploidentical (haplo) donor HCT in the setting of post-transplant cyclophosphamide (PTCy). In addition, haplo donor recipients showed a higher risk of viral and fungal infections, hemorrhagic cystitis, cardiovascular toxicities, and delayed immune reconstitution. This research suggests that HLA-matched donors should be prioritized over mismatched donors when available.
The use of PTCy for GVHD prevention has expanded options for patients. Several studies have compared haplo related donor HCT using PTCy to matched related and MUD HCT using traditional calcineurin inhibitor GVHD prophylaxis. Outcomes were reported to be similar in both groups but did not include use of a uniform GVHD prophylaxis strategy.
This retrospective study reviewed the outcomes of haplo, MUD, and MSD HCT recipients who received PTCy as GVHD prevention. The study’s purpose was to evaluate the impact of HLA matching in PTCy-based GVHD prophylaxis by comparing matched graft sources (related and unrelated) to haplo HCT performed within a single institution.
This single center study (MD Anderson Cancer Center, The University of Texas) of 661 adult patients included 275 haplo, 246 MUD, and 140 MSD patients who received a first allogeneic HCT using PTCy and tacrolimus (Tac) with or without mycophenolate mofetil (MMF) between January 2015 and July 2020. The median age in the haplo group was 51 years old, but 60-61 years old in the other groups. The most common diagnosis was acute myeloid leukemia (AML) or myelodysplastic syndrome (MDS) in all groups. More patients in the haplo group (76%) received reduced intensity conditioning (RIC) than other groups (26-40%). Almost all MSD and three-quarters of the MUD received peripheral blood (PB) grafts, while a majority of haplo (66%) received bone marrow (BM). The median follow-up was 17, 29, and 30 months in the haplo, MUD, and MSD groups.
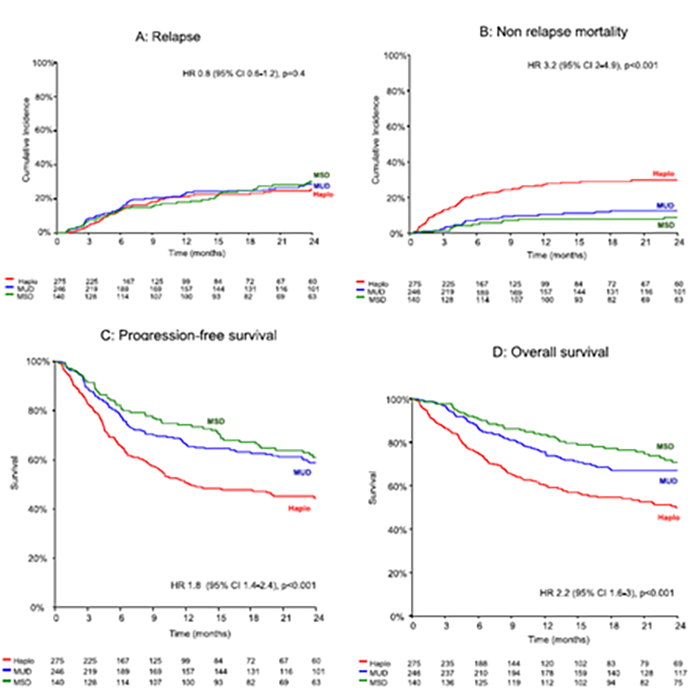
Results showed the MUD and MSD groups had significantly better overall survival, progression-free survival, and non-relapse mortality than the haplo group. Haplo was associated with a higher risk of infections, adverse complications, and delayed immune reconstitution, which may have contributed to the higher risk of non-relapse mortality. Relapse rates were not different between groups.
These results support findings from prior studies that HLA-matched donors are associated with better outcomes to mismatched donors in PTCy-based GVHD prophylaxis. The National Marrow Donor Program®/Be The Match® is committed to expanding further research regarding HLA-matched and mismatched donor outcomes to maximize access to transplant.
Figures 1A-1D. Clinical Outcomes
Mehta R, et al., published in Transplantation and Cellular Therapy
