Expanding donor registry models to include mismatched unrelated donors (MMUD) down to a 5/8 HLA match expands access to nearly 100% of patients in need of hematopoietic stem cell transplantation (HCT). That’s according to research presented at the 2022 Tandem Meetings of the American Society of Transplantation and Cellular Therapy (ASTCT) and the CIBMTR® (Center for International Blood and Marrow Transplant Research®). Based on the availability of alternative graft sources and advances in graft-versus-host disease (GVHD) prophylaxis following allogeneic HCT, MMUD has the potential to expand HCT access, particularly among racially and ethnically diverse patients.
Download a PDF of the study highlights and citation here.
Not all patients in need of unrelated donor allogeneic HCT will have a fully (8/8) matched donor available. The likelihood of a match varies substantially based on a patient’s racial or ethnic background, with Black and African American patients having only a 29% chance of finding an 8/8 matched, available donor on the Be The Match Registry®. Recent observational studies and clinical trials (Shaw et al., 2021) have highlighted the safe and effective use of MMUD in the setting of post-transplant cyclophosphamide and other novel GVHD prevention strategies that allow for expanded donor choice and optimization of other donor selection characteristics, including donor age. Tools to rapidly assess unrelated donor search productivity can help guide clinical decision making.
Using registry modeling techniques previously developed at the National Marrow Donor Program® (NMDP)/Be The Match®, researchers evaluated the likelihood of finding a donor in the Be The Match Registry for 21 detailed race/ethnic groups considering high resolution matching at 8/8, 7/8, 6/8, and 5/8 levels using 2020 donor registry population characteristics. Registry data was adjusted for demonstrated donor availability. Race/ethnic groups examined were as follows: African American, African, South Asian Indian, American Indian – South or Central American, Alaska Native or Aleut, North American Indian, Caribbean Black, Caribbean Hispanic, Caribbean Indian, Filipino, Hawaiian or Other Pacific Islander, Japanese, Korean, Middle Eastern or North Coast of Africa, Mexican or Chicano, European Caucasian, Chinese, Hispanic – South or Central American, Black – South or Central American, Southeast Asian, and Vietnamese.
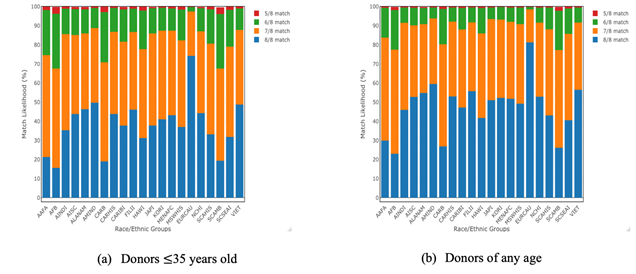
The results in the figure below show the match likelihoods for each race/ethnic group. The likelihood of an 8/8 match ranges from 74% to as low as 16%; however, when allowing for HLA match levels down to 5/8, such availability becomes greater than 99% for all race/ethnic groups, even when restricting to donors 35 years old or younger.
These registry models demonstrate the potential for use of MMUD at different HLA match levels to increase access to transplant for all patients, including those who are racially and ethnically diverse. Expanded donor options also allow for further selection of desirable MMUD non-HLA characteristics demonstrated by the nearly 100% availability of donors 35 years old or younger for all groups. Innovative transplant approaches that permit use of MMUD and other HLA mismatched donors hold the potential to erase the gap in donor availability for all populations.
Match Likelihoods for Each Race/Ethnic Group
Chowdhury AS, et al., Tandem poster abstract
