According to research published in Bone Marrow Transplantation by the Acute Leukemia Working Party of the European Blood and Marrow Transplant Group (EBMT), patients who received a single antigen mismatched (9/10) unrelated donor hematopoietic stem cell transplant (MMUD HCT) had better outcomes than those who received a haploidentical donor (haplo) HCT. These results suggest that less HLA mismatching is associated with better outcomes following allogeneic HCT using post-transplant cyclophosphamide (PTCy) based graft-versus-host disease (GVHD) prophylaxis.
The use of PTCy for GVHD prevention has extended use of multiple-mismatched haplo related donor HCT. This GVHD prophylaxis approach is also being applied for MMUD HCT. Therefore, this study was designed to compare outcomes between 9/10 MMUD to haplo HCT using PTCy. Finding superior outcomes in single antigen MMUD HCT could expand donor options and access for patients in need of HCT.
This study included 1,751 adult patients 18 years old or older, with 155 patients receiving 9/10 MMUD peripheral blood (PB) stem cell grafts (1-agMMUD-PB), 647 patients receiving haplo bone marrow (Haplo-BM), and 949 patients receiving haplo PB grafts (Haplo-PB). The patients received a first allogeneic HCT using PTCy-based GVHD prophylaxis between January 2009 and September 2019 as reported to the EBMT. Haplo-PB patients were older, with a median age of 55 years, compared to 52 years in both 1Ag-MMUD-PB and Haplo-BM (p < 0.01). The median time from diagnosis to transplantation was 6 months in all groups, showing no time-to-transplant advantage for haplo over MMUD.
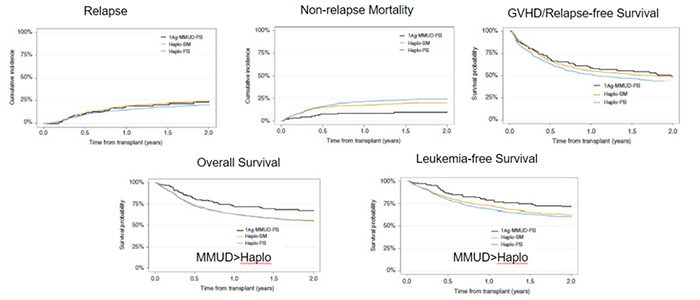
The results show better overall survival, non-relapse mortality, and leukemia-free survival outcomes in the 9/10 MMUD patients than in the Haplo-BM and Haplo-PB patients (see Figure 1 below).
In context with prior studies demonstrating superior outcomes with matched graft sources (matched related and unrelated) compared to increasing mismatched haplo donors, this data suggests the impact of HLA matching may fall along a continuum, and prioritization of less mismatched unrelated donors may be preferable to haplo. Mismatching with unrelated donor sources may be a better option for patients than previous data suggests, which could provide more opportunities for patients without suitable related donors.
Figure 1. Clinical Outcomes for 9/10 MMUD vs. Haplo HCT
Battipaglia G, et al., published in Bone Marrow Transplantation
