In the United States, 25 to 80% of patients with hematologic malignancies lack an HLA-matched (8/8 alleles) unrelated donor for hematopoietic cell transplantation (HCT) despite international registries listing more than 38 million volunteer donors. The greatest disparities are present in access for patients who are ethnically diverse.
The study conducted between December 2016 and March 2019 in 11 transplant centers enrolled 80 patients to assess the safety and efficacy of MMUD (4/8 – 7/8) HCT. The patients were divided evenly into two groups: 40 receiving the myeloablative and 40 receiving reduced intensity HCT with bone marrow (BM) as a graft source. Approximately half of the study participants were ethnically diverse which is consistent with expectations based on donor availability within registries. Patients with a suitable HLA matched related or URD were excluded and the regimen intensity was at the center’s discretion.
The aim was to determine 1-year overall survival (OS) after HLA MMUD bone marrow transplantation using PTCy, sirolimus and MMF to prevent GVHD. Patients received a fresh BM graft, followed by PTCy on days +3, +4, and sirolimus/MMF starting on day +5. The goal was to achieve a 1-year survival after HLA MMUD bone marrow transplantation of 65% or higher—similar to the 1-year survival observed after HLA haploidentical related donor HCT using bone marrow as the graft source.
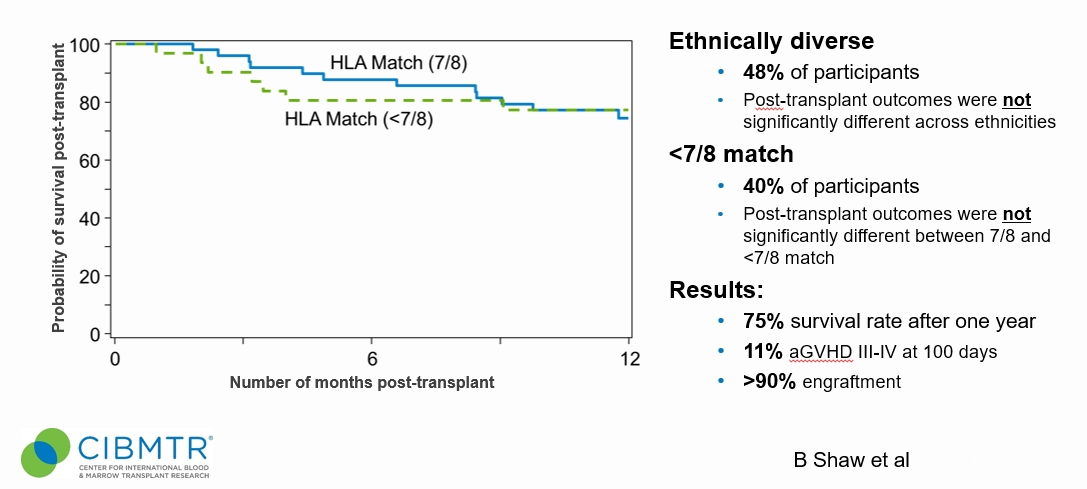
The secondary hypotheses were that greater than 90% of the individuals would engraft and the incidence of grades III-IV GVHD would be less than 15% at day +100. The results were encouraging with a 75% survival rate after 1 year, over 90% engraftment, and a 11% rate of aGVHD III-IV at 100 days. The study population was composed of nearly 50% ethnically diverse patients and nearly 40% of the cohort received <7/8 matched HCT.
Selecting a MMUD may have benefits over a haplo donor, such as removing risk associated with donor specific antibodies and allowing for preferential selections of other favorable donor factors like younger age. The researchers concluded expanding access to HCT, especially for patients who are ethnically diverse, using MMUDs is feasible as the outcomes of using MMUDs in the setting of PTCy are similar to those obtained using a haplo donor.