This CIBMTR® (Center for International Blood and Marrow Transplant Research®) analysis examined racial and socioeconomic outcome disparities among long-term allogeneic hematopoietic cell transplant (HCT) survivors. Results indicate no significant link between race/ethnicity, neighborhood poverty level and long-term outcomes following HCT.
Download a PDF of the study highlights and citation.
These findings, while running counter to previous research, draw attention to the necessity for enhanced monitoring for post-transplant complications and emphasize the need for improved care systems for survivors to ensure equity in outcomes.
Background
Historically, patients who are racially and ethnically diverse, particularly those in higher-poverty neighborhoods, have shown poorer post-HCT survival compared to non-Hispanic White counterparts and those without socioeconomic challenges. Such differences have often been attributed to race, socioeconomic status (SES) and insurance type. Previous research from the CIBMTR highlighted that African Americans experienced reduced overall post-HCT survival compared to non-Hispanic White patients, with both African Americans and Hispanics facing heightened non-relapse mortality (NRM) rates. To further explore these disparities, the current study centered on long-term survivors.
Study Details
Using the CIBMTR database, this research included 5,473 first-time allogeneic HCT recipients in the U.S. from 2007 to 2017, all of whom were over 18 years old at the time of their transplant and had sustained a remission status for at least a year post-HCT. The study included patients diagnosed with acute myeloid leukemia (AML), acute lymphoblastic leukemia (ALL), chronic myeloid leukemia (CML) or myelodysplastic syndrome (MDS). The study included all graft sources, donor sources and conditioning regimens.
Results
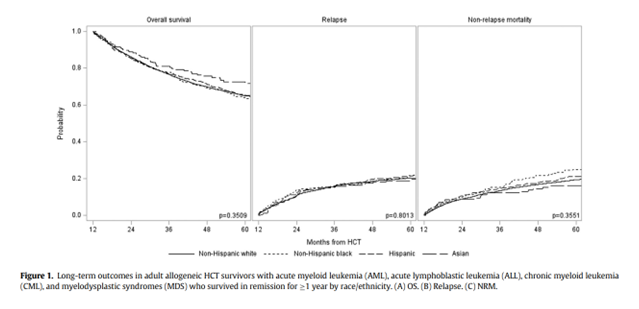
The 5-year overall survival (OS) rates were distinct among races with Asians leading at 74%, Hispanics at 70%, and both non-Hispanic Whites and Blacks at 65%. Asians exhibited the lowest cumulative incidence of NRM at 13%, followed by Hispanics at 16%, non-Hispanic Blacks at 20%, and non-Hispanic Whites at 21%. The median post-transplant follow-up durations varied among the different racial groups with 69 months for non-Hispanic Whites, 50 months for non-Hispanic Blacks, 59 months for Hispanics, and 57 months for Asians.
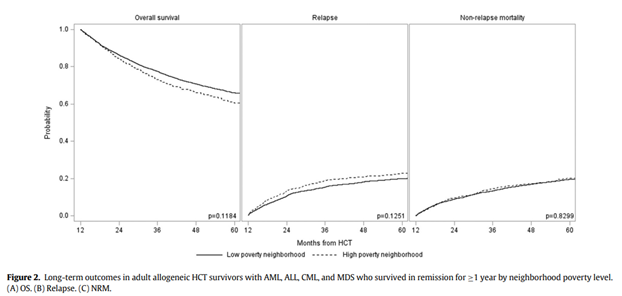
After multivariable analyses, there were no discerned disparities in OS or NRM across racial or ethnic groups. However, the type of residence (urban/rural) and insurance emerged as significant factors affecting OS and NRM. Specifically, rural inhabitants and those insured under Medicaid or Medicare faced heightened mortality risks. Causes of death remained consistent across racial and ethnic boundaries, disease relapse was the predominant cause, followed by GVHD, infections, and organ failures. Interestingly, the cohort's mortality rates were approximately 10 times higher than their general population counterparts, with notable racial and ethnic variations.
Key Takeaways
Among the adult allogeneic HCT recipients who achieved a minimum of 1 year in remission following HCT, there appeared no significant associations between race/ethnicity, neighborhood poverty strata and long-term outcomes—a contrast to some preceding studies. This underlines the importance of monitoring post-transplant complications, necessitating comprehensive screening, proactive prevention, and immediate, guideline-based management.
The study also illuminates the need to innovate care models and infrastructures. This could encompass survivorship care plans, telemedicine, and web-integrated self-management platforms, which are pivotal for ensuring the well-being of long-term survivors, especially those not in direct connection with or proximity of their transplant centers.
Blue BJ, et al., Published in Transplantation and Cellular Therapy
