This study analyzed the effects of publicly reporting center-specific survival analysis (CSA) scores, which reflect the 1-year overall survival rates of patients after allogeneic hematopoietic cell transplantation (alloHCT) at various United States transplant centers. The findings revealed that transplant centers with a negative CSA score (indicating worse survival outcomes) saw an 8-9% reduction in patient volume the following year, while neighboring centers saw a 3.5% increase.
These findings suggest that publicly reported CSA scores may produce unintended consequences that could potentially restrict access to care, prompting further investigation into the causes and implications of these volume shifts.
Download a PDF of the study highlights and citation here.
Background
In response to the Transplant Amendments Act of 1990 and the Stem Cell Therapeutic and Research Act of 2005, the CIBMTR® (Center for International Blood and Marrow Transplant Research®) has been responsible for the public reporting of alloHCT outcomes at U.S. transplant centers since 2010. The CIBMTR's CSA predicts and reports the 1-year overall survival (OS) rate for each center based on several risk factors.
Previous research has indicated that reporting on center performance in the context of solid organ transplantation was associated with low-performing transplant centers experiencing a decline in transplant volumes over time. Therefore, this study was initiated to examine if CSA reporting impacts patient volumes at transplant centers for alloHCT.
Study Details
Out of 203 U.S. transplant centers reporting data to the CIBMTR during the study, 91 were included in the analysis. Those 91 centers actively treat adult or combined adult and pediatric populations, had reported CSA scores, and performed a minimum of 10 alloHCTs each year from 2012 to 2018. The analysis excluded autologous HCTs and CAR-T cell therapy infusions.
Factors considered in the study included prior year transplant center volume, previous year CSA score, CSA score changes from two years prior, calendar year, center type (adult-only vs. combined adult and pediatric), and years of alloHCT experience.
Results
Among the included transplant centers, 68 experienced at least one change in their annual CSA score. Centers with a CSA score of -1 (underperforming) experienced an 8-9% reduction (p <0.001) in mean alloHCT volume the following year compared to those with a score of 0 (performing as expected) or +1 (performing better than expected).
Centers neighboring a transplant center with a -1 CSA score saw a 3.5% increase in mean alloHCT volume (p=0.04). These changes, suggesting the migration of alloHCT volumes, persisted for up to 2 years following a transplant center being classified as underperforming.
Key Takeaways
The study suggests that public reporting of CSA scores may correlate with changes in the volumes of alloHCT at transplant centers. There is an ongoing investigation into the various reasons behind these volume shifts and their impacts on patient outcomes.
The study highlights the need to be aware of the after-effects of CSA reporting, such as potentially limiting access to HCT due to perceived suboptimal performance at specific centers. Patients should be empowered to choose the transplant center that is the best fit for them. Tools, navigation, and community hematology/oncology providers should be used to help patients get the best care when they need it in an accessible way.
Figure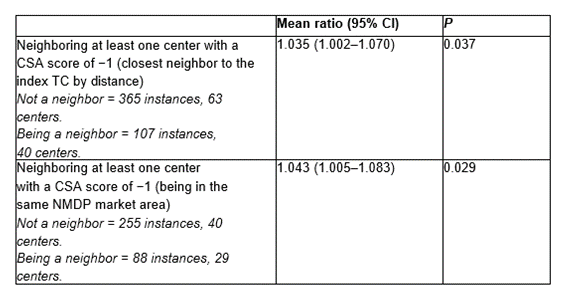
Sharma A, et al., Published in Transplantation and Cellular Therapy
