According to research published in Blood Advances, structural racism is the key factor accounting for health disparities among racially and ethnically diverse patients with acute myeloid leukemia (AML). The novel structural racism variable assessed using census tract data in this study accounted for nearly all Black-White and Hispanic-White disparity in AML survival. These findings show structural racism to be a stronger mediator of survival disparities than comorbidities, molecular features of the AML, health care access, and treatment.
Download a PDF of the full study summary with journal citation here:
Non-Hispanic Black (NHB) and Hispanic patients with AML have higher mortality rates than non-Hispanic white (NHW) patients despite more favorable disease genetics and younger age at diagnosis. While acknowledging that census-level data is a narrow indicator of structural racism, this study is the first attempt to objectively examine and operationalize structural racism—defined by racial segregation, disadvantage, and affluence at the census tract level—as a determinant of inequities in acute leukemia outcomes. Structural racism refers to systematic disadvantages experienced by certain groups of people. Although racial and socioeconomic differences have been identified as prognostic factors in many solid organ malignancies, their impact on hematologic cancers is understudied.
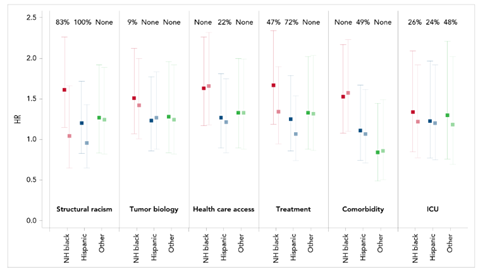
This multilevel analysis reviewed six composite variables, including defined census tract disadvantage and tract affluence calculations. The variables included structural racism, tumor biology, healthcare access, comorbidities, treatment patterns, and intensive care unit (ICU) admission during induction chemotherapy. Researchers performed the analysis to determine the extent of how tract-level socioeconomic status (SES) and segregation led to outcome disparities for NHB and Hispanic patients more generally. Models adjusted for age, sex, and study site, compared with NHW patients.
The patient cohort of 822 adults diagnosed with AML from January 2012 through January 2018 were split into four groups categorized by race/ethnicity: NHB, Hispanic, NHW, and other racial/ethnic groups. The median patient age was 62 years old.
Tract disadvantage as part of the structural racism variable included the proportion of:
- Families with incomes below the poverty line
- Families receiving public assistance
- Adults that were unemployed
- Households that were female-headed households with children
Another component of structural racism, tract affluence, was defined as the proportion of:
- Families with incomes greater than $75,000
- Adults with at least a college education
- Adults employed in professional or managerial occupations
Based on mediation analysis, variables intended to serve as proxies for structural racism (tract disadvantage, tract affluence, tract proportion NHB, tract proportion NHW) appeared to account for nearly all the AML survival disparity in this study. Variables representing tumor biology (ELN prognostic score and secondary leukemia) did not appear to mediate racial/ethnic disparities in leukemia death, either individually or when modeled together. Health care access variables accounted for one-fifth of the Hispanic-NHW disparity, but not in other groups.
Leukemia death was significantly greater for NHB patients (hazard ratio [HR] 1.59) compared to Hispanic patients (HR 1.25) and patients of other races/ethnicities (HR 1.34). NHW patients were more likely to live in affluent areas, have private insurance, and receive a transplant. NHB patients were more likely to live in less affluent areas, have an adverse-risk disease, and exhibit higher-risk molecular features of disease and mutations of AML. NHB patients were also less likely to have a transplant than all other patient groups.
Hispanic patients showed similar transplant access to NHW. However, they were less likely to have insurance and live in affluent areas. Leukemia death was higher for all patients residing in more disadvantaged and less affluent areas, patients residing in areas with a greater proportion of NHB residents, patients with secondary AML, patients with higher-risk disease, and patients admitted to the ICU.
This study shows that the way structural racism was constituted, the variable accounts for nearly all the disparity seen in AML outcomes for racially and ethnically diverse patients. There is a need to develop interventions to reduce disparities in AML mortality, specifically for underserved populations.
The National Marrow Donor Program®/Be The Match®, alongside the CIBMTR® (Center for International Blood and Marrow Transplant Research®), is committed to expanding access to all patients who need HCT. Engagement between community hematology/oncology practices and transplant centers fosters collaboration to identify structural racism barriers to treatment and develop interventions for practice change.
Figure 1. Disparity of Hazard Ratio in Leukemia Death
Abraham I, et al., published in Blood Advances
