The purpose of this study was to compare haploidentical (haplo) to HLA-matched unrelated donors (MUD) and examine the impact of donor age and type on the outcomes of patients with acute myeloid leukemia (AML). Patients in complete remission (CR) received reduced-intensity conditioning hematopoietic cell transplantation (RIC-HCT) with post-transplant cyclophosphamide (PTCy) graft-versus-host disease (GVHD) prophylaxis.
Download a PDF of the study highlights and citation here.
Both younger and older haplo transplants were associated with significantly inferior overall survival (OS) and higher non-relapse mortality (NRM) compared to younger MUD transplants. The older haplo group also demonstrated a significantly higher risk of acute GVHD.
These results suggest a preference for younger MUD over haplo donors in adult patients with AML undergoing RIC-HCT with PTCy GVHD prophylaxis.
Background
This research was motivated by the need to improve HCT outcomes in AML patients. Despite PTCy being a standard prophylaxis strategy for GVHD, previous data showed patients receiving haplo HCT had higher risks of acute GVHD, NRM, and inferior OS than those receiving MUD HCT.
Previous studies comparing MUD and haploidentical donors did not fully consider the donor's age, which is known to impact HCT outcomes. Therefore, the researchers decided reanalyze a publicly available CIBMTR® (Center for International Blood and Marrow Transplant Research®) dataset to compare HCT outcomes between younger and older haplo and MUD donors to assess if donor age influences these outcomes, with the hypothesis that younger haplo donors might lead to comparable OS as younger MUD donors.
Study Details
The study included patients with AML (n=775), grouped based on their donors: younger MUD (less than 35 years; n=84), younger haplo (less than 35 years; n=302), and older haplo (greater or equal to 35 years; n=389). Most patients were male, and peripheral blood was the most commonly used graft source, particularly in the MUD group. Haplo groups were more ethnically diverse, and a higher proportion received a fludarabine, cyclophosphamide, and total body irradiation regimen than the MUD group. The median follow-up was approximately 24 months across all groups.
Results
This study reported the highest 3-year OS in the younger MUD group (68.5%), compared to the younger (50.8%) and older (42.2%) haplo groups. Both haplo groups displayed significantly higher NRM and inferior OS than the younger MUD group, with the highest NRM observed in the older haplo group (22.0%).
The older haplo (33.7%) group exhibited a higher risk for acute GVHD than the younger haplo (25.8%) and younger MUD (20.2%) groups. Still, no significant differences were seen in chronic GVHD rates. Infections and causes of death did not vary significantly between the groups, although fungal infections were more common in the older haplo group. The older haplo group had a higher risk of NRM and acute GVHD than the younger haplo group, without significant differences in relapse or OS. See the Figure below for results.
Key Takeaways
This study shows that in patients with AML undergoing RIC-HCT with PTCy for GVHD prevention, use of a younger MUD resulted in lower complications and higher survival rates than haplo donors, irrespective of their age. Furthermore, older haplo donors were associated with higher rates of acute GVHD than younger MUDs. No significant differences were observed in relapse rates or chronic GVHD across the groups.
These results suggest that for adult patients with AML in remission, younger MUDs may be preferred over haplo donors. These findings provide guidance for health care providers to help their patients with the best treatment options.
Figure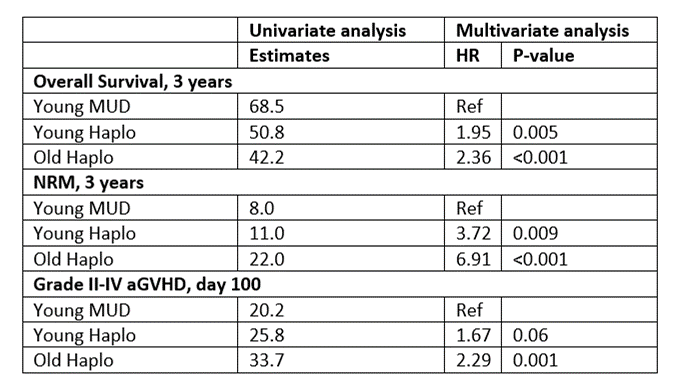
Mehta R, et al., Published in Transplantation and Cellular Therapy
