Studies presented at the 2023 Tandem Meetings of the ASTCTTM and the CIBMTR® compared the outcomes after allogeneic hematopoietic cell transplantation (alloHCT) based on donor type for patients with acute myeloid leukemia (AML) and B-cell acute lymphoblastic leukemia (B-ALL). Patients who received alloHCT using an older matched sibling donor (MSD) had a significantly higher 5-year relapse rates than those who used a younger matched unrelated donor (MUD).
Background
The incidence of ALL and AML is increasing in adults. AlloHCT offers a cure for patients with ALL or AML, but disease relapse remains a significant issue. MSD has been considered the ideal donor type in clinical practice due to the lower risk of graft-versus-host disease (GVHD) and improved disease-free survival (DFS). However, with aging patients, their siblings are also likely to be older and have more comorbidities. Additionally, adults with ALL or AML often undergo reduced-intensity conditioning (RIC) and need novel strategies to reduce post-alloHCT relapse risk.
Recent data have suggested relapse reduction and DFS benefits from using a younger MUD for patients with myelodysplastic syndromes, but the impact in adult ALL and AML patients remains unknown.
Study Details
Two retrospective studies using CIBMTR registry data included patients aged 50 and older undergoing alloHCT from 2011 through 2018. The first study included patients with B-ALL (n=925). The second study included patients with AML (n=4,684). Patients received either an older MSD (50 years and older) or younger MUD (35 years and younger) alloHCT.
The study populations included the use of bone marrow and peripheral blood grafts, RIC or myeloablative conditioning regimens, and most patients received calcineurin inhibitor based GVHD prophylaxis. The primary outcome was relapse risk, and secondary outcomes were non-relapse mortality (NRM), DFS, and overall survival (OS).
Results
The 5-year disease relapse for B-ALL patients was significantly higher in recipients of older MSD HCT than younger MUD HCT (37% vs. 26%). The NRM for B-ALL patients was higher in the younger MUD group than in the older MSD group (31% vs. 22%). Neither the DFS nor OS had a statistically significant difference between both groups as shown in Figure 1.
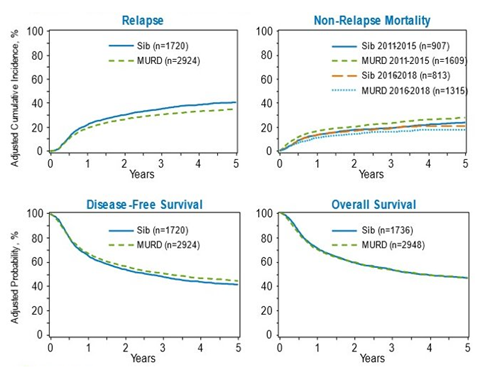
AML patients had a higher 5-year relapse among recipients of older MSD HCT compared to younger MUD HCT (41% vs. 35%). The NRM for AML patients varied by the time frame they received alloHCT. Patients receiving alloHCT between 2011 and 2015 had a significantly higher NRM in the younger MUD group than in the older MSD group (28% vs. 24%). Those receiving alloHCT between 2016 and 2018 did not show a statistically significant difference in NRM between the younger MUD and MSD groups as shown in Figure 2 (17% vs. 20%, p=0.147).
Key Takeaways
These studies showed a significant relapse reduction in B-ALL and AML patients who received alloHCT with a younger MUD compared to an older MSD. The results suggest that younger MUD may lead to a more substantial graft-versus-leukemia effect and may be preferred in donor selection over an older MSD, especially for patients at high risk of post-alloHCT relapse.
Further research is needed to determine if higher NRM in younger MUD may be mitigated with advances in GVHD prevention strategies, such as post-transplant cyclophosphamide, combined with other supportive care measures.
Figure 1. 5-Year B-ALL Outcomes
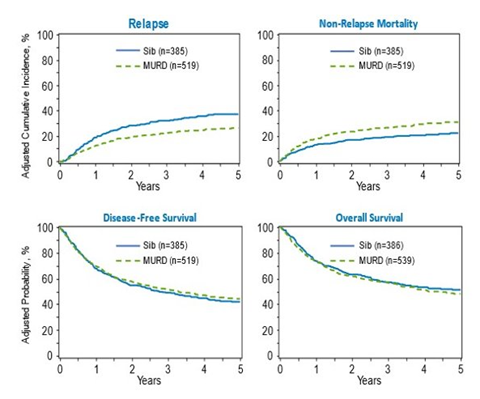
Figure 2. 5-Year AML Outcomes
Abid MB, et al., ALL Study Tandem Abstract
Abid MB, et al., AML Study Tandem Abstract
